Written by: Erika Swant, MPH, RDN Candidate (@theforkingdietitian)

1. Prepare for longggg journey.
Breastfeeding can be hard! This is something that most women don’t know before they start. You have to prepare not only with required materials, but also mentally.
How long do you want to breastfeed for? Set a goal and make a plan of how you are going to stick with it. The American Academy of Pediatrics and CDC recommend that infants be exclusively breastfed for about the first 6 months. From 6 months to one year, breastfeeding is recommended along with the introduction of complementary foods for one year or longer. WHO differs in that they recommend complimentary breastfeeding up to 2 years of age or longer.¹ Whatever you decide is best for you and your baby, make a plan that will encourage your short-term and long-term goals.
After you set your goals, figure out who your support system will be. Will it be family members or friends that have breastfed? Maybe it will be a breastfeeding support group. Whichever it is, it will be nice to have a safe place to get your questions answered.
2. Breastfeeding Survival Kit
Here are some important things* you should have ready before giving birth. Think about creating your own kit:
- Breast pump (some insurances will cover this)
- Milk storage bottles or bags
- Milk storage space organizer
- Nursing pillow
- Nursing cover, if you roll that way
- Nursing bra
- Breast pads for leakage
- Cooling gel pads for sore nipples
- Nipple cream or balm – and lots of it!
This is not an all inclusive list, however, it is a good start to prepare for your breastfeeding journey. Depending on your situation, a breast pump is a good thing to have on hand. Along with this, storage for milk and a way to keep your pumping dates and times organized is a must!
A nursing pillow will help support your baby and make it easier for them to reach your breast. A nursing cover is nice if you are out and about and would like some privacy. However, all moms across the country have the legal right to publicly breastfeed!
And for you, mama! When purchasing nursing bras, think about waiting until the last couple of weeks of your pregnancy journey. This will ensure that you still have a fitting bra postpartum. When your milk comes in, your breasts may be even bigger, so keep these things in mind while making these purchases. Additionally, nipple creams and gel pads are great products for dry or cracked nipples.
3. Take a Breastfeeding Class
Breastfeeding classes can help get you into the mindset that this is truly a journey between you and your baby. Here are some things a breastfeeding class may help with:
- Understand the benefits of breastfeeding
- Understand how breastfeeding works
- Learn how your breasts produce milk
- Understand milk composition throughout the day
- What nutrients don’t get passed through milk (iron)
- How to establish a healthy supply of breastmilk
- How to help the baby latch
- How to know if the baby is getting enough milk
- Different breastfeeding positions
- Understand the many reasons your baby may want to breastfeed
- Who to call for help
- Increasing confidence – You go mama!
If you cannot afford a breastfeeding class, you can check with WIC to see if you are eligible or find a breastfeeding support group online. Either way, try to do some research on each of these topics beforehand so you feel confident and prepared!
In addition to prenatal nutrition education, I have an entire video-based module on breastfeeding and postpartum resources in my Pregnancy Nutrition Vault!
4. When you get to the hospital: make it very clear you are breastfeeding.
Being very clear about your expectation to breastfeed can help ensure that alternative options will not be pushed onto you and your baby. Hospitals or birthing centers may try to give you formula samples, but being very clear that you are breastfeeding will let them know you are determined and motivated to make breastfeeding work for you.
5. Ask for lactation support at the hospital!
If something isn’t working out for you such as the baby’s latch or milk expression, let the healthcare team know that you’d like to speak to a lactation specialist. Lactation consultants are experts within this area and can help you get on the right path before leaving the hospital. This will help you make sure everything is off to a solid start and will help minimize pain or soreness that comes with breastfeeding.
6. Make a plan for when things…crack.
Something that isn’t typically talked about is how breastfeeding hurts. Some women only experience this at the beginning and some throughout their entire breastfeeding journey. Just remember this is normal! Your nipples are not used to this continuous stimulation. What you can prepare for however, is what you will do when it is enough to throw the towel in.
A proper latch is the best way to prevent soreness. Again, making sure you check in with a lactation consultant before you leave the hospital will help ensure that your baby is latching properly. Additionally, nipple cream, gel pads, and even just putting some milk on your nipples before and after breastfeeding can help prevent dryness.
Another tip is to avoid washing your nipples with soap! A warm rinse with water will be sufficient in order to allow the Areolar Glands to function properly. These glands are most important for releasing a natural, oily substance that contains antibacterial properties, which will help from getting infected (mastitis).²
Lastly, follow up with your support system! Anybody you know who has already breastfed or any support groups you are in can help answer any questions or give you tips.
7. Don’t expect to be on a schedule right away
Your baby will dictate their feeding schedule! This is tough at first, but remember that babies have the innate instinct of hunger and they can let you know when it is time to eat. Also keep in mind that your baby may not only want to eat when they’re hungry, but also maybe when they are sick, scared, have trouble sleeping, or when they just need some comfort. And this is okay too! Since they are feeding on cue, this could also help with your milk supply as your milk increases with demand.
Some signs your baby may be hungry include their fists moving toward their mouth, “rooting” or their head moving toward your breast, sucking on hands or lip smacking, becoming more alert or active, and opening or closing their mouths.³ These are signs that you may catch before they start crying, which will help mom’s sanity and baby’s stress!
8. Know which nutrients are not passed through breastmilk, what to eat etc.
Two micronutrients to keep in mind for breastfed infants are vitamin D and iron.
Unfortunately, even if mom is taking vitamin D, it isn’t sufficient for the baby. An infant supplement is an easy fix since most infants will need this right after birth to avoid becoming deficient. The American Academy of Pediatrics recommends that breastfed or partially breastfed infants have about 400IU of vitamin D each day starting within the first few days of life.⁴
Most newborns have sufficient iron stored from birth. However, this is typically depleted at 4 months of age. At 4 months, you can start supplementing 1 milligram of iron for each kilogram of body weight.⁴ Once your baby starts solids, you can start feeding foods that are high in iron, such as fortified baby cereal or infant meats!
Check out my *Amazon Store for my top supplement recommendations.
9. Learn how not to cry over spilt milk.
Let’s be real, moms have the right to cry over spilt milk. Breastfeeding is hard and you don’t want to see any of that hard work go down the drain – literally.
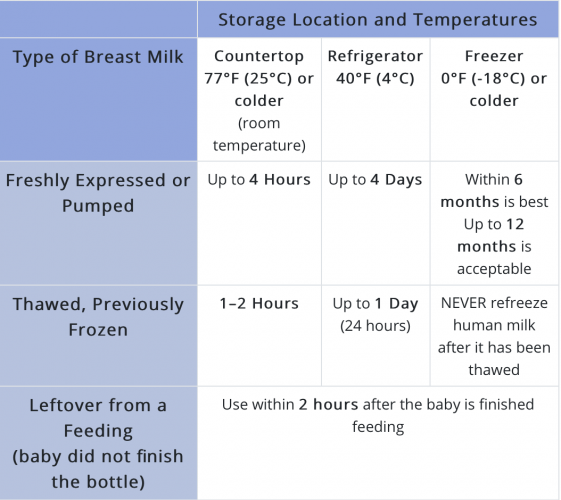
Here are some tips for storing breastmilk and how to decrease waste. The CDC has provided this straightforward table.
Image Reference: https://www.cdc.gov/breastfeeding/recommendations/handling_breastmilk.htm
If a feeding is technically expired, DON’T throw it out! You can use expired milk in a milk bath. Just remember to label it, so you don’t get it mixed up.
Resources:
- CDC. “Frequently Asked Questions (FAQs).” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 28 May 2020, www.cdc.gov/breastfeeding/faq/index.htm#howlong.
- Doucet S, Soussignan R, Sagot P, Schaal B. The secretion of areolar (Montgomery’s) glands from lactating women elicits selective, unconditional responses in neonates. PLoS ONE. 2009;4(10):e7579. doi:10.1371/journal.pone.0007579
- WIC. “Baby’s Hunger Cues.” Baby’s Hunger Cues | WIC Breastfeeding, wicbreastfeeding.fns.usda.gov/babys-hunger-cues.
- CDC. “Iron.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 21 Sept. 2020, www.cdc.gov/breastfeeding/breastfeeding-special-circumstances/diet-and-micronutrients/iron.html.
*This post contains Amazon affiliate links. I make a small commission off qualified purchases.
The post 9 Tips to Prepare for Breastfeeding appeared first on marissamccormick.com.